Discipline : Haematology
Definition
Can be classified by aetiology:
Primary : autoimmune disorder characterised by isolated thrombocytopenia (most common)
Secondary : secondary to identifiable trigger: - Autoimmune disorders : SLE, Antiphospholipid syndrome - Malignancy: Lymphoma, Leukaemia (particularly CLL) - Infection: HIV, HCV - Drugs: many check AMH
Can be classified by chronicity:
Newly diagnosed ITP : all cases <3 months of diagnosis
Persistent ITP : ITP lasting 3-12 months
Chronic ITP : ITP lasting >12 months
Epidemiology
US Statistics:
- Females affected more than males
- highest prevalence <5 years old; typically self-limiting after viral infection; 80% resolve in 12 months
- highest prevalence in >55 years old; often incidental finding on routine CBC
Pathophysiology
- Antiplatelet antibodies (mostly IgG directed against GpIIb/IIIa, GpIb/IX, bind to surface proteins on platelets → sequestration by spleen and liver → ↓ platelet count → ↑ bone marrow megakaryocytes and platelet production)
Clinical Features
- Splenomegaly is typically absent in patients with ITP@1709712278047
- Clinical features can correlate with platelet count; but most patients are asymptomatic:
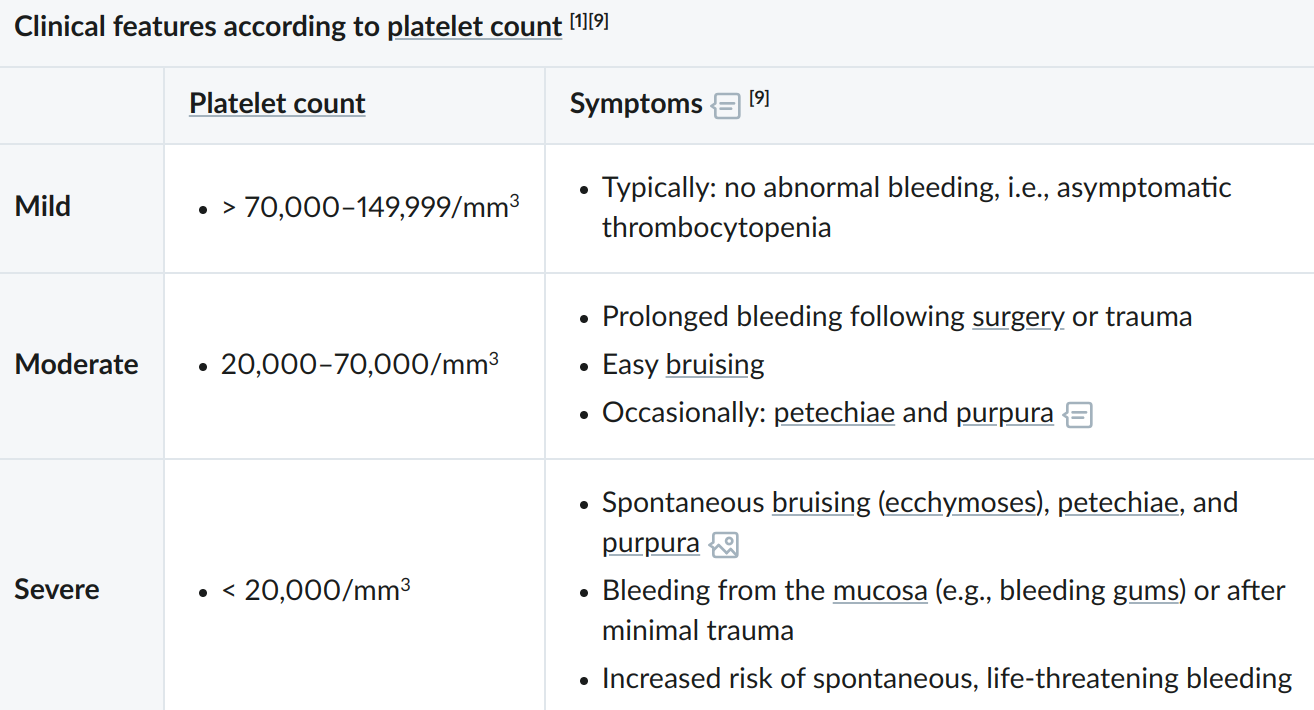
- Minor mucocutaneous bleeding is possible:
- Subcutaneous: bruising, petechiae, purpura
- Mucosal: mild epistaxis, gingival bleeding
Investigations
CBC : Typically <
Coagulation panel is usually normal (unless secondary)
Bleeding time may be prolonged
Consider additional investigations for secondary causes: (e.g. HIV and HCV screening)
Bone marrow biopsy : normal or ↑ megakaryocytes
Diagnosis
- ITP is often a diagnosis of exclusion in patients who have thrombocytopenia with no other abnormalities
Management
- In all patients stop medications that impair platelet function (e.g. NSAIDs)
Emergency Treatment
Indicated for patients with:
- Life threatening bleeding (typically at platelet )
- Acute neurological features (i.e. intracranial bleed)
- Anticipated urgent surgery or invasive procedure
Emergenct Management:
- Haemostatic control of bleeding (if present)
- Start combination therapy with:
- Corticosteroids (e.g. methylprednisolone)
-
- IV immunoglobulin
-
- Platelet transfusions as needed
- If ⌀ response consider thrombopoietin receptor agonist (TPO-RA) e.g. romiplostim
Conservative Managmenet
Indicated for asymptomatic or minor mucutaneous bleeding only patients with:
- Adults with a platelet count
- Children with any platelet count
Remember to refer to haematology and counsel on bleeding risks1
First Line Medical Therapy
Indicated for:
- Adults with platelet count
- Patients with significant non-life-threatening mucosal bleeding (e.g. severe epistaxis)
- Symptoms impacting quality of life
Therapy:
- Corticosteroids (e.g. dexamethasone or prednisone)
- If contraindicated or not tolerated: IVIG or anti-Rho(D) immunoglobulin
Therapy for ITP Refractory to First-Line or Persistent/Chronic ITP
- TPO-RAs (e.g. Romiplostim, Eltrombopag)
- Rituximab
- Splenectomy
- Indications:
- Treatment resistent thrombocytopenia lasting >12 months
- Severe bleeding refractory to other treatment
- Spleen should be confirmed as primary site of platelet breakdown using radioactively labeled thrombocytes if possible
- Indications:
Additional Flashcards
When to suspect ITP
Text
Suspect c1::ITP in a child with thrombocytpoenia and petechiae following a viral illness
Source
Amboss: Immune thrombocytopenia. Accessed 6 March 2023 available at: https://next.amboss.com/us/article/8q0OZh#Ld8fe0f824fb313404f48b4e9850945ec
Emergency management
Text
What is the emergency management for ITP once haemostatic control is achieved?
c1::Corticosteroids c1::IVIG c1::Platelet transfusions as needed
Extra
If ⌀ response consider thrombopoietin receptor agonist (TPO-RA)
Source
Amboss: Immune thrombocytopenia. Accessed 6 March 2023 available at: https://next.amboss.com/us/article/8q0OZh#Ld8fe0f824fb313404f48b4e9850945ec
One by one
y
First line therapy
Text
First line therapy for ITP is with c1::corticosteroids (e.g. dexamethasone or prednisone)
Extra
Indicated for:
- Adults with platelet count
- Patients with significant non-life-threatening mucosal bleeding (e.g. severe epistaxis)
- Symptoms impacting quality of life
Source
Amboss: Immune thrombocytopenia. Accessed 6 March 2023 available at: https://next.amboss.com/us/article/8q0OZh#Ld8fe0f824fb313404f48b4e9850945ec
Footnotes
-
Advised to avoid contact sports and other high-risk activities ↩